
Introduction
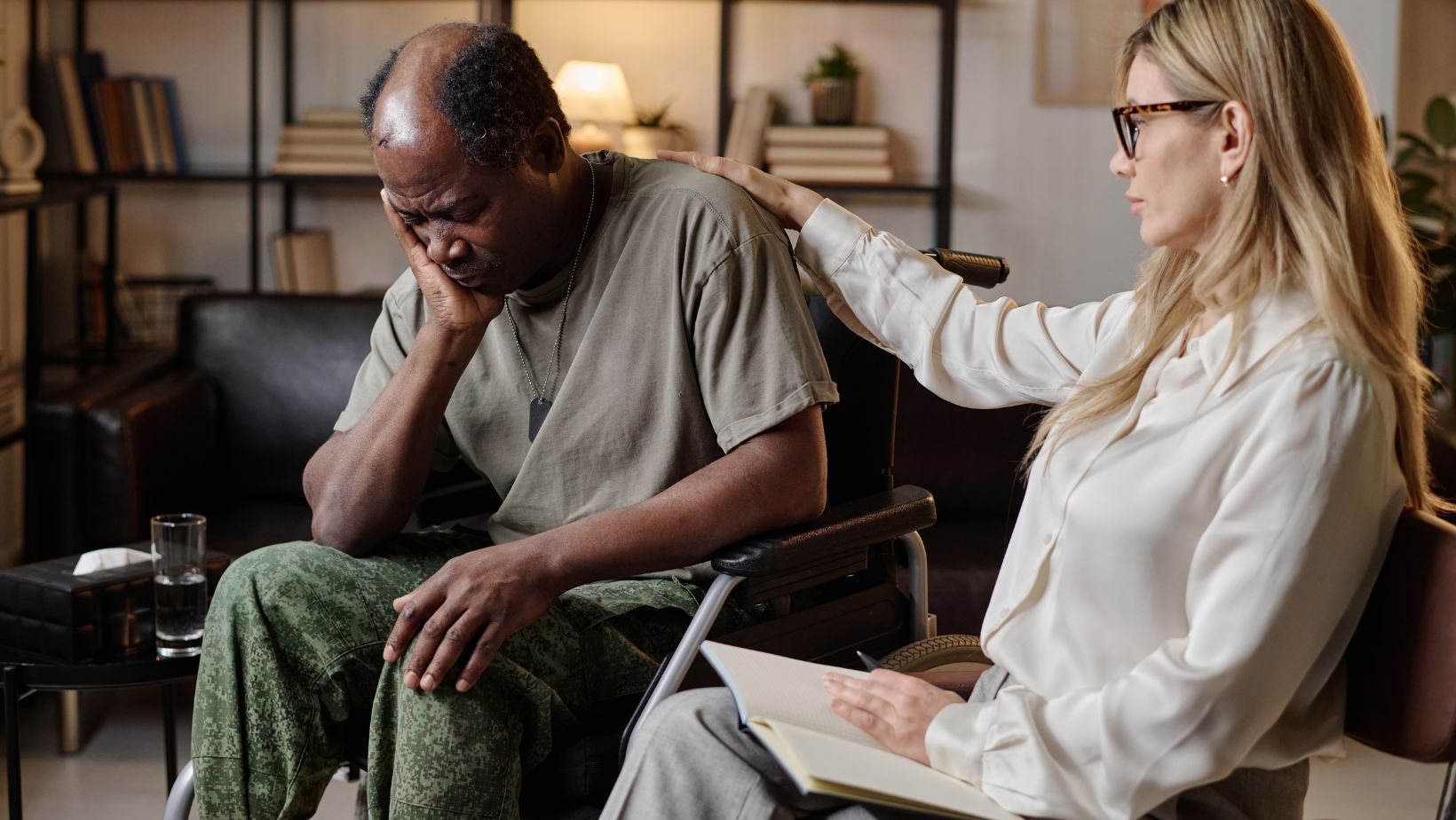
Veterans face unique mental health challenges as a result of their military service, and these challenges often continue long after they leave active duty. The transition from military to civilian life can be difficult, and many veterans struggle with trauma, anxiety, depression, and other mental health issues. Recognizing and addressing the mental health needs of veterans is essential to ensure that those who have served receive the care and support they deserve.
In this article, we will explore the specific mental health needs of veterans, the common conditions they face, and how families, communities, and healthcare providers can offer the support necessary for their well-being.
The Mental Health Challenges Faced by Veterans
Military service can be both physically and mentally demanding. For many veterans, the stress of combat, the loss of fellow service members, or even the daily rigors of military life can leave lasting emotional scars. While some veterans reintegrate into civilian life smoothly, others face significant mental health struggles.
Post-Traumatic Stress Disorder (PTSD)
One of the most common mental health conditions among veterans is Post-Traumatic Stress Disorder (PTSD). PTSD occurs after experiencing or witnessing traumatic events such as combat, violent conflicts, or life-threatening situations. Veterans with PTSD may experience flashbacks, nightmares, emotional numbness, and hypervigilance, making it difficult for them to feel safe or at ease in everyday situations.
According to the U.S. Department of Veterans Affairs (VA), 11-20% of veterans who served in Operations Iraqi Freedom (OIF) and Enduring Freedom (OEF) experience PTSD in any given year. For veterans of the Vietnam War, the number is estimated to be around 15%.
Depression
Depression is another mental health condition that affects a significant number of veterans. The loss of purpose, difficulty adjusting to civilian life, and unresolved trauma can all contribute to feelings of sadness, hopelessness, and a lack of interest in previously enjoyable activities. Depression can interfere with daily functioning, relationships, and career aspirations, making it harder for veterans to move forward in their post-military life.
Anxiety and Panic Disorders
For many veterans, the stress of military service leads to chronic anxiety or panic disorders. This anxiety can manifest as constant worry, irritability, restlessness, or difficulty concentrating. Veterans may also experience panic attacks, which involve sudden, intense episodes of fear accompanied by physical symptoms like a racing heart, shortness of breath, or sweating.
The National Center for PTSD notes that veterans are more likely than the general population to suffer from anxiety disorders, often as a result of combat-related trauma.
Substance Abuse
Veterans may turn to substances like alcohol or drugs as a way to cope with the emotional pain of their experiences.
Substance abuse is often a way to numb feelings of anxiety, depression, or trauma, but it can lead to addiction, further complicating mental health recovery. The Substance Abuse and Mental Health Services Administration (SAMHSA)reports that 1 in 15 veterans had a substance use disorder in the past year, making this a significant issue within the community.
Suicidal Thoughts and Behaviors
The combination of PTSD, depression, and substance abuse can lead to an increased risk of suicide among veterans. Tragically, many veterans feel that they have no way out of their emotional pain. According to the VA’s 2020 National Veteran Suicide Prevention Annual Report, veterans are 1.5 times more likely to die by suicide than non-veteran adults, highlighting the critical need for effective mental health intervention.
Barriers to Seeking Mental Health Support
Despite the high rates of mental health issues among veterans, many do not seek the help they need. Several barriers contribute to this gap in care, including stigma, a lack of accessible resources, and difficulties transitioning to civilian life.
Stigma Around Mental Health
For some veterans, there is a cultural stigma attached to seeking mental health treatment. Military culture often emphasizes strength, resilience, and self-reliance, and admitting to mental health struggles can feel like a sign of weakness. Veterans may fear being judged by others or may not want to acknowledge their emotional pain, leading them to avoid seeking professional help.
Limited Access to Care
While there are healthcare services available to veterans, many face challenges in accessing these services, especially in rural areas or if they lack reliable transportation. Long wait times, complicated bureaucratic processes, or a lack of nearby mental health professionals can prevent veterans from receiving timely and effective care. This can result in veterans going untreated or delaying care until their symptoms worsen.
Difficulty Transitioning to Civilian Life
The transition from military service to civilian life can be disorienting for veterans. They may struggle to find employment, adjust to new social norms, or feel disconnected from the civilian community. This disconnection can make it difficult for veterans to feel understood or supported, further complicating their mental health recovery.
Addressing the Mental Health Needs of Veterans
Given the unique mental health challenges veterans face, it is crucial to provide comprehensive support that meets their emotional, psychological, and practical needs. There are several ways to support veterans as they navigate their mental health journey.
Provide Access to Veteran-Specific Mental Health Services
Veterans often benefit from veteran-specific mental health services provided by professionals who understand the unique experiences of military life. The VA offers a variety of mental health programs tailored to veterans, including counseling for PTSD, depression, and substance abuse. Community-based organizations like Veterans of Foreign Wars (VFW) or The American Legion also provide resources and support networks that can help veterans feel understood and cared for. Clinics like Veterans Punta Cana offer specialized care for U.S. veterans living abroad, providing access to mental health services and support in a familiar, veteran-focused setting.
Encourage Peer Support Networks
Veterans who connect with others who have shared similar experiences may find a greater sense of community and understanding. Peer support groups, whether through the VA or other veteran organizations, provide a safe space for veterans to talk openly about their struggles and learn from others who have faced similar challenges. Peer support can be a valuable tool in reducing feelings of isolation and providing encouragement on the path to recovery.
Promote Mental Health Education and Awareness
Raising awareness about mental health and reducing the stigma around seeking help is essential for ensuring veterans get the care they need.
Educating veterans about the signs of mental health issues, such as PTSD, anxiety, or depression, can empower them to seek help early. At the same time, encouraging open conversations about mental health in the military and veteran communities can reduce the stigma and promote a culture of support and understanding.
Improve Access to Care
Expanding access to mental health services for veterans is critical. This includes improving VA services, offering telehealth options for veterans in remote areas, and ensuring that mental health care is affordable and easily accessible. Reducing wait times, simplifying the process of obtaining care, and providing transportation options for veterans who need to travel to appointments can help address these barriers.
Support Family Involvement
Families often play a crucial role in a veteran’s mental health recovery. Providing families with education on how to support their loved ones and access mental health services can make a significant difference. Involving family members in counseling sessions or support groups can foster better communication and strengthen the support network around the veteran.
Conclusion
The mental health needs of veterans are complex and often shaped by the experiences they had during their military service. From PTSD and depression to anxiety and substance abuse, veterans face unique challenges that require specialized care and support. By addressing the stigma around mental health, improving access to care, and fostering community and peer support, we can help veterans navigate the difficult journey of mental health recovery. Veterans have given so much in service to their country, and it is our responsibility to ensure they receive the care and understanding they deserve.












