
Taiwan’s medical device regulatory framework is designed to ensure that all products entering its market meet rigorous safety, efficacy, and quality standards. Overseen by the Taiwan Food and Drug Administration (TFDA) under the Ministry of Health and Welfare (MOHW), the system requires pre-market approval for every class of medical device. Whether you are a domestic manufacturer or an international company looking to commercialize your device in Taiwan, understanding the regulatory landscape is essential. Moreover, compliance with Quality System Documentation (QSD)—akin to Good Manufacturing Practices—is a prerequisite for registration. For foreign manufacturers, appointing a local agent is mandatory to manage the registration process and ensure continuous liaison with the TFDA. This article will explore the classification process, registration pathways, documentation requirements, and the role of local representation in achieving successful medical device market entry in Taiwan.
Classification of Medical Devices in Taiwan
Understanding the Classification System
The classification system is designed to align with the inherent risk a device may pose to patients and users.
- Class I Devices: These devices are subject to a more streamlined regulatory process, often relying on a self-declaration or simplified notification procedure, which minimizes administrative burdens while still ensuring compliance with essential quality controls. Manufacturers are expected to maintain consistent good manufacturing practices and adhere to basic standards that ensure product safety. Despite their low-risk designation, oversight remains vital to prevent any compromise in device performance. This category is designed to facilitate innovation and market entry for straightforward medical devices while maintaining a fundamental level of safety and effectiveness. Continuous quality improvement remains a priority, ensuring that even low-risk devices deliver dependable clinical performance.
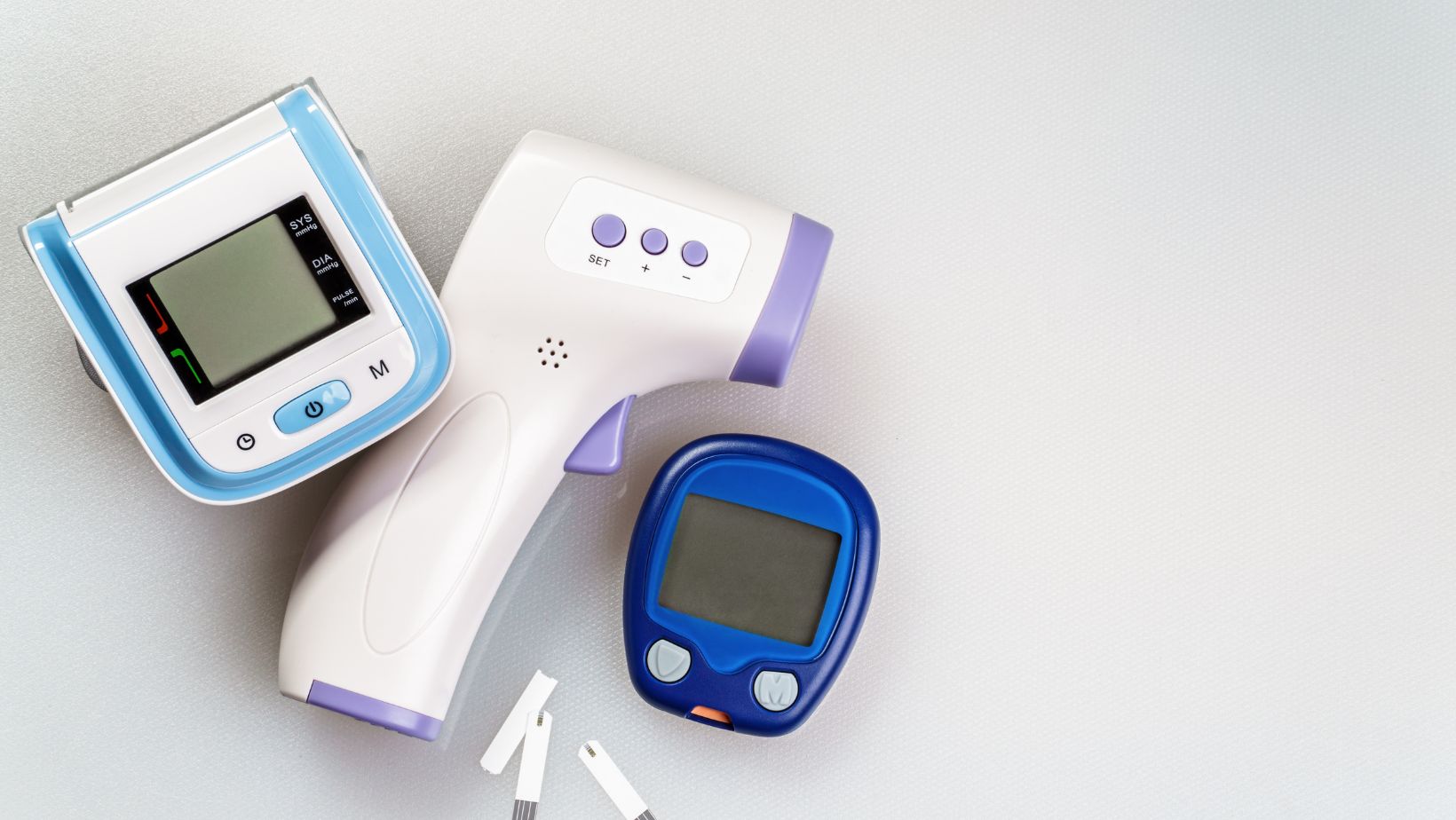
- Class II Devices: Class II devices fall within the moderate-risk category and typically contain more complex diagnostic equipment or devices that have a direct impact on patient management, such as blood pressure monitors and certain imaging systems. The regulatory process for these devices is more comprehensive than that for Class I, requiring manufacturers to compile detailed technical documentation, performance test reports, and sometimes preclinical data to substantiate safety and efficacy. In addition, these devices often necessitate prior approval in the manufacturer’s home country, which serves as an initial validation of their quality and performance. This tier of regulation is designed to ensure that any device with moderate risk is thoroughly evaluated, thereby offering a balanced approach that promotes innovation while protecting patient health. Rigorous oversight in this category helps to maintain a high standard of clinical performance and reliability.
- Class III Devices: The registration process for these devices is exceptionally stringent, involving comprehensive technical documentation and extensive clinical evidence to verify safety and effectiveness. Manufacturers must demonstrate robust compliance with advanced Quality System Documentation requirements, which serve as a testament to the device’s reliability and the manufacturer’s commitment to excellence. This level of regulation is necessary to mitigate the risks associated with complex medical interventions, ensuring that any potential hazards are carefully controlled. The intensive review process underscores the importance of patient safety and clinical efficacy, demanding that manufacturers provide substantial data and validation before these critical devices can be approved for use.
- New Devices: New devices refer to products that do not have an established predicate approved by the regulatory authority, necessitating an even more detailed and rigorous review process. These devices undergo comprehensive evaluations to assess their safety and effectiveness from the ground up, often involving additional preclinical or clinical investigations. The absence of a direct predicate requires manufacturers to furnish extensive technical and scientific evidence, demonstrating that the innovative device meets all relevant regulatory standards. This pathway is designed to foster innovation by allowing novel products to enter the market while ensuring that they are thoroughly scrutinized for potential risks. Enhanced review procedures provide a framework that encourages technological advancement and maintains the highest patient protection standards.
By tailoring the regulatory process to the complexity and potential hazards associated with different devices, authorities can protect public health while promoting innovation and technological progress.
Criteria for Classification
The classification is based on several factors, including:
- Intended Use and Indications for Use: The intended use and indications for use of a device form the cornerstone of its classification, as they define the primary function and clinical applications of the product. In this context, regulators closely examine whether the device is meant for diagnosis, treatment, monitoring, or supportive roles during medical procedures. The clarity of the intended purpose is critical, as it directly influences the level of scrutiny and risk assessment applied. A device intended for a simple monitoring task may be subject to less rigorous evaluation compared to one designed for direct therapeutic intervention. Additionally, the documented clinical indications help determine how the device fits within existing treatment paradigms and whether it offers a distinct advantage over current standards of care.
- Technological Characteristics: The technological characteristics of a device are integral to its classification, as they reveal the complexity and innovativeness of its design. This evaluation focuses on both the sophistication of the engineering and the novelty of the underlying technology. Devices incorporating cutting-edge materials, unique software algorithms, or advanced diagnostic capabilities may be subject to additional scrutiny. Regulatory authorities assess whether the technology represents a significant departure from existing products, particularly in cases where there is no clear predicate device. The evaluation process includes an in-depth review of design specifications, manufacturing processes, and potential integration with other systems. Such an assessment helps determine whether the innovative aspects of the device justify a higher risk category, thereby necessitating more extensive clinical validation and quality assurance measures.
- Risk to the Patient or User: Evaluating the potential risk to patients or users is a critical factor in the classification process, as it directly influences the level of regulatory oversight required. This criterion involves an analysis of the device’s invasiveness, potential for adverse events, and the likelihood of complications during use. Devices that involve surgical implantation or those that require direct interaction with sensitive biological tissues naturally command a higher level of risk assessment. Regulators examine historical data, preclinical studies, and clinical trial results to determine the extent of any risks associated with the device. The goal is to ensure that potential hazards are adequately identified and mitigated through design features or enhanced safety protocols.
- Regulatory Precedents: Regulatory precedents play a significant role in the classification of medical devices, as they offer a historical context that informs current decision-making. By reviewing similar devices that have already been approved locally or internationally, regulators can leverage prior experiences to streamline the assessment process. This involves comparing technical specifications, safety profiles, and clinical outcomes to establish a benchmark for the new device. When a device closely resembles a previously approved product, it may benefit from a more expedited review process, assuming that the predicate device demonstrated satisfactory performance and safety. On the other hand, if a device diverges significantly from established norms, a more rigorous evaluation might be necessary. Such precedents help reduce uncertainty in regulatory decisions and ensure consistency in classifying devices.
Together, they form a comprehensive framework that ensures medical devices are appropriately evaluated and safely integrated into clinical practice. This balanced methodology protects patients and fosters a regulatory environment that supports continued innovation and improvement in healthcare technologies.
Registration Process and Documentation Requirements for Medical Devices in Taiwan
Once a medical device has been correctly classified, manufacturers must navigate the detailed registration process required by the Taiwan Food and Drug Administration (TFDA).
Pre-Market Approval Submission
For all classes of devices, pre-market approval is mandatory before they can be sold in Taiwan. The submission begins with preparing an application form and supporting documents detailing the device’s technical specifications, intended use, and manufacturing process. For Class I devices, a simplified submission—often referred to as a self-declaration or notification—is sufficient, while Class II and III devices require a much more extensive dossier. For devices classified as New (with no predicate), additional scrutiny is applied as the TFDA must establish safety and effectiveness from scratch.
Dossier Compilation
The dossier must include a wide range of documents:
- Technical Documentation: Technical documentation is the foundation of the dossier, detailing the product’s design, intended use, and intricate component structure. This section requires thorough descriptions that cover product drawings, engineering specifications, and the underlying technology that drives the device’s functionality. Manufacturers must provide clear narratives that explain the device’s construction, materials, and operational mechanisms. Where applicable, referencing previously approved predicates can assist in contextualizing the device’s performance within established frameworks, potentially simplifying the review process. Emphasis is placed on transparency and detail to ensure that regulatory reviewers have all necessary technical insights to assess compliance with safety and performance standards. The documentation must articulate the device’s design evolution and demonstrate how each component contributes to its overall effectiveness.
- Testing and Validation Data: Testing and validation data play a pivotal role in establishing the safety and performance characteristics of the device. This dossier section requires comprehensive test reports that contain preclinical evaluations and, if necessary, clinical trial data. Manufacturers need to present methodologically sound studies that detail how the device meets or exceeds established performance criteria. Data should include detailed protocols, test conditions, results, and analyses that validate the device’s functionality under varied scenarios. For devices with moderate risk classifications, approvals from recognized international bodies like those in the US or EU might be referenced, while higher-risk or innovative devices demand more rigorous testing. The validation process ensures that the device performs reliably and safely, thereby supporting a robust regulatory review. Documentation should also discuss any observed variances and the corrective measures taken to address them.
- Labels and Instructions for Use: Labels and instructions for use are integral to ensuring that end users receive clear and accurate guidance on device operation. This portion of the dossier must include all Chinese language versions of labels, packaging inserts, and instructional materials. Detailed content is required to describe the proper use, handling precautions, storage conditions, and maintenance procedures associated with the device. The documents must be crafted to meet local regulatory language requirements and cultural considerations, providing comprehensive user support. Clarity in these materials is essential to minimize user errors and enhance patient safety. Additionally, the documentation should outline the process by which these materials were developed and validated, ensuring that they reflect the most current safety standards and practical usage information.
- Authorization and Supporting Certificates: The final section of the dossier compiles all necessary authorization documents and supporting certificates that establish the device’s legitimacy in the market. Foreign manufacturers are required to include a letter of authority from the originating manufacturer, a Free Sales Certificate (FSC) from the relevant health authority, and, where applicable, additional documentation such as a truth and accuracy statement or manufacturer’s license. This collection of documents serves as an endorsement of the device’s quality and market approval in its country of origin. It provides the regulatory body with assurances that the device has been subject to rigorous oversight and adheres to international standards. These supporting certificates are indispensable for confirming the device’s track record and facilitating its acceptance in Taiwan.
Each component—from technical documentation to authorization certificates—plays a vital role in demonstrating that the device meets all safety, quality, and performance standards. A well-prepared dossier expedites the regulatory review and builds a robust case for market acceptance.
Submission and Review Timeline
After submission, the TFDA conducts an administrative review to ensure that all documents are complete and properly formatted. For Class I devices, the review can be relatively swift—often within one month—whereas Class II and III devices can take anywhere from 5 to 15 months, depending on complexity and additional data requirements. Manufacturers are encouraged to maintain close communication with their appointed local agent, who acts as the liaison with TFDA, to promptly address any deficiencies or additional requests during the review process.
Post-Approval Surveillance
Once a device is approved, it is issued a “medical device permit license” that is valid for a set period, typically five years. However, approval does not mark the end of regulatory obligations. Manufacturers must continue to comply with post-market surveillance requirements, including adverse event reporting, periodic safety updates, and product recalls when necessary. This ongoing commitment helps ensure that devices remain safe and effective throughout their lifecycle. Manufacturers can effectively navigate Taiwan’s registration pathway by meticulously compiling the necessary documentation and adhering to the TFDA’s structured review process, ultimately ensuring that their products meet the high standards demanded by the Taiwanese market.
Local Representation and Quality System Documentation Compliance
The Role of a Local Agent
A local agent serves as a bridge between the foreign manufacturer and the TFDA. Their responsibilities include preparing and submitting registration dossiers, facilitating communication during regulatory reviews, and assisting with any post-market surveillance activities. This representative not only streamlines the submission process by ensuring that all documents are accurately translated into Chinese but also helps to address any questions or additional information requests issued by the TFDA. The local agent is pivotal in navigating complex regulatory landscapes and expediting the overall approval timeline by maintaining a strong relationship with regulatory authorities. Furthermore, their knowledge of domestic market trends, regulatory updates, and procedural nuances can give manufacturers strategic insights that lead to more efficient product launches. They often assist in identifying potential challenges early on, advising on the best practices for dossier preparation, and even recommending changes to product labeling or documentation to align with TFDA expectations.
Quality System Documentation (QSD) Compliance
Quality System Documentation (QSD) is critical to Taiwan’s regulatory framework. It serves as Taiwan’s version of Good Manufacturing Practice (GMP) and ensures that the manufacturing facilities of medical device companies adhere to stringent quality standards. All manufacturers, except for certain low-risk, non-sterile Class I devices, are required to secure a QSD certificate before or concurrently with their product registration. This certificate verifies that the manufacturer’s quality management system complies with both international standards, such as ISO 13485, and additional Taiwan-specific requirements.
Achieving QSD compliance involves a rigorous audit of the manufacturing facility. The process includes a comprehensive review of production processes, equipment maintenance, document control procedures, and overall quality control systems. Manufacturers must provide detailed documentation that illustrates every aspect of their production process—from raw material sourcing to final product inspection. In cases where a manufacturer holds an ISO 13485 certificate issued by one of the six TCP III approved Notified Bodies, this can often be leveraged to expedite the QSD review process. However, the TFDA may require additional evidence or clarification to confirm that all local regulatory criteria are met.
Navigating the medical device registration process in Taiwan requires a comprehensive understanding of classification criteria, detailed documentation requirements, and the indispensable role of local representation. Manufacturers must invest significant effort in preparing extensive dossiers that include technical documentation, performance test reports, and Quality System Documentation (QSD) to meet the TFDA’s rigorous standards. With the regulatory framework designed to safeguard public health and ensure product safety, foreign companies must partner with experienced local agents who can bridge language barriers, facilitate communication with regulatory authorities, and help streamline the approval process.













