Pain is an experience we all share in one way or another, but its nature is far from simple. From a stubbed toe to chronic pain conditions, pain signals are complex and influenced by both physical and psychological factors. So, how does our body modulate these signals? Why do we sometimes feel pain more intensely, or other times, less so? Let’s explore the fascinating mechanisms that govern how the body modulates pain and the different ways it can be managed.
The Complexity of Pain Perception
Pain doesn’t just occur when we’re injured. It’s a sensory experience that begins when nociceptors, the nerve receptors for pain, are activated due to injury, inflammation, or environmental stimuli. These nociceptors send pain signals to the brain, where they’re processed and interpreted.
However, the body’s perception of pain can be influenced by many factors, from physical conditions to psychological states. Pain isn’t merely a one-way communication from body to brain; it involves intricate mechanisms that allow our bodies to manage and modify pain.
How the Body Modulates Pain
Our bodies have several natural systems that can adjust the intensity of pain we experience. One well-known mechanism is the release of endorphins, which are neurochemicals that act as natural painkillers. Activities like exercise, laughter, or even eating certain foods can trigger the production of these chemicals, offering relief from pain and creating a sense of euphoria.
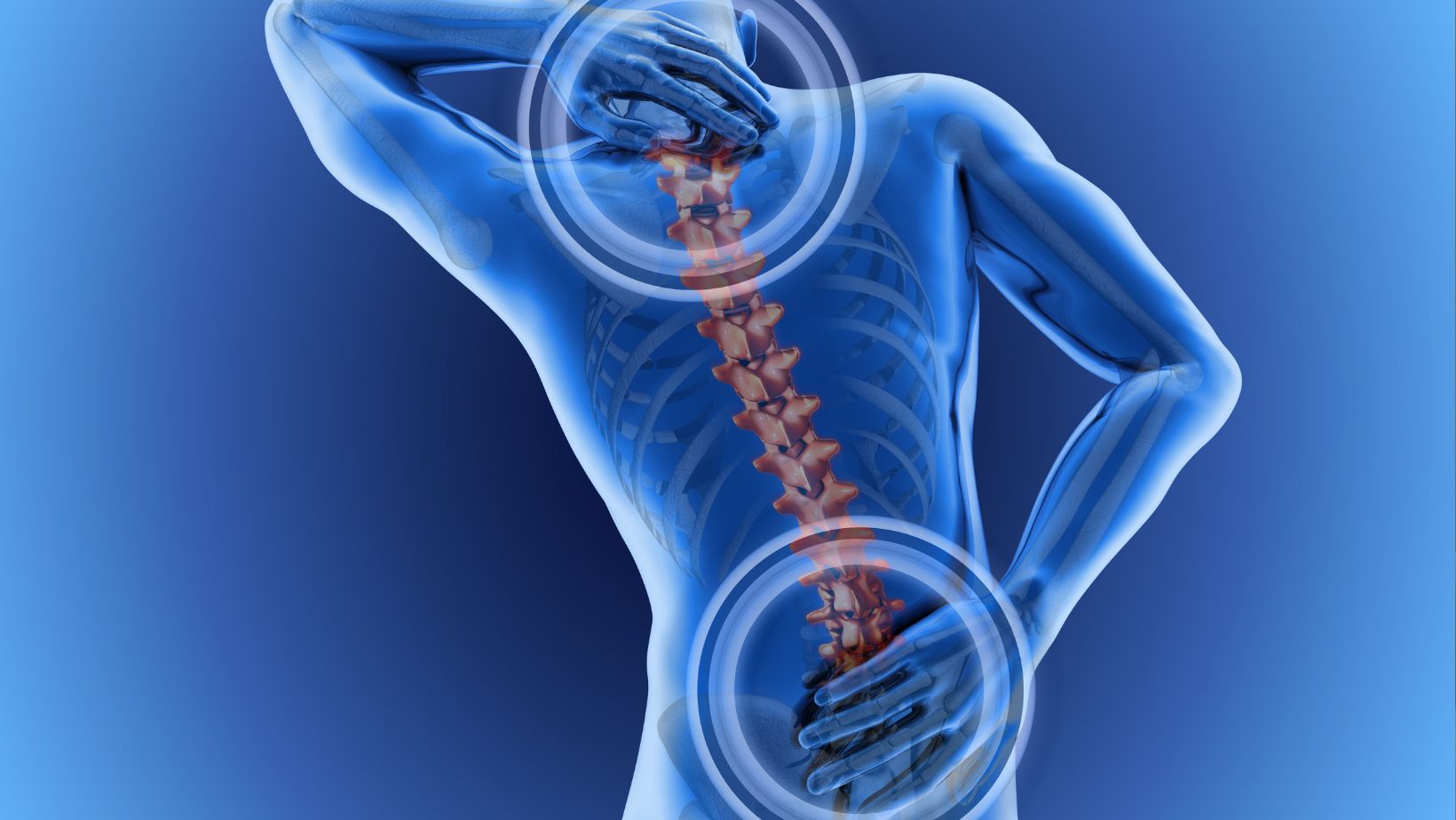
Another important system in pain modulation involves descending pathways from the brain to the spinal cord. In these pathways, the brain can send signals down to dampen pain, particularly when the body is under stress or in danger. This mechanism helps the body manage pain in high-adrenaline situations, where it may be beneficial to not focus on pain until the threat is over.
One of the most intriguing processes in pain modulation is what is described by the pain gate theory. This theory proposes that there is a “gate” in the spinal cord that regulates how much pain signal is allowed to pass through to the brain. Sensory signals like touch, pressure, or warmth can influence this gate and either close it or open it, depending on the situation. For instance, rubbing a sore area can block pain signals from reaching the brain by stimulating non-painful touch receptors, effectively closing the gate.
The Role of Psychology in Pain Perception
Psychological states greatly influence how we process and experience pain. For instance, stress and anxiety can make pain feel more intense. When stressed, the body releases higher levels of cortisol, a stress hormone that can increase muscle tension and heighten the sensation of pain. This is why pain often feels worse when we’re anxious or under pressure.
Conversely, mental relaxation can diminish pain. Techniques like mindfulness, meditation, and breathing exercises help calm the nervous system, which in turn lowers pain sensitivity. This is why some people with chronic pain conditions report relief through psychological therapies or relaxation techniques.
Additionally, cognitive conditions, such as ADHD, can affect how pain is perceived. People with ADHD may experience heightened sensitivity or reduced awareness of pain due to differences in how their brain processes sensory input. This can lead to an altered pain experience, where the body might amplify or suppress pain signals in response to the unique cognitive patterns found in different ADHD Types.
Physical Health and Lifestyle: Their Impact on Pain Modulation
Physical health plays a significant role in how pain is managed. Regular exercise is one of the best ways to modulate pain because it stimulates the production of endorphins, which reduce pain perception. Physical activity also improves circulation, reduces inflammation, and strengthens the body, all of which contribute to less frequent or intense pain episodes.
Sleep and nutrition are also critical. Poor sleep and unhealthy eating habits can exacerbate pain, while proper rest and a balanced diet help maintain a healthy nervous system. Chronic pain conditions, like arthritis or fibromyalgia, often involve the central nervous system becoming hypersensitive, making pain more persistent even when there is no ongoing injury.
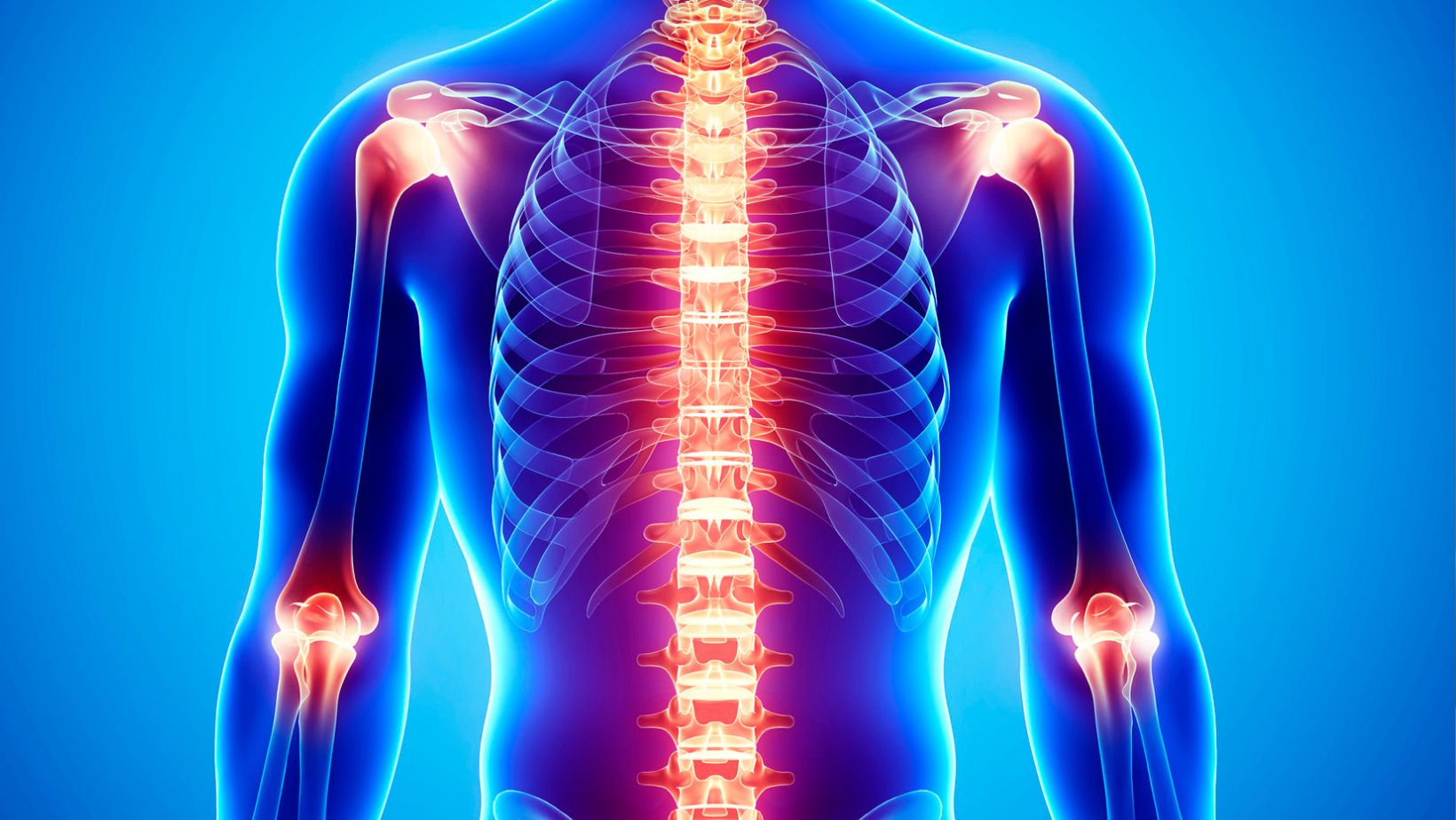
Chronic Pain and Central Sensitization
In conditions like neuropathic pain or fibromyalgia, the pain modulation system becomes disrupted, leading to central sensitization. This means the nervous system becomes overactive, and pain signals continue to be sent to the brain, even after the initial cause of pain has healed. In chronic pain conditions, this heightened sensitivity results in the body continuously perceiving pain, even when it should no longer be present.
Central sensitization is one of the reasons why managing chronic pain can be so challenging. It means that pain isn’t just a result of an injury—it becomes a condition in itself, where the body’s pain perception system is malfunctioning.
Pain Management: Modern Approaches and Treatments
Pain management today is multi-faceted, offering a combination of medical, physical, and psychological treatments to address pain on various levels. Conventional methods like pain medications, including NSAIDs and opioids, provide immediate relief but come with risks and side effects, particularly when used long-term. As a result, many people turn to alternative and complementary treatments for more sustainable pain management.
TENS therapy (Transcutaneous Electrical Nerve Stimulation) is a common neuromodulation technique that uses electrical impulses to interfere with pain signals, effectively “closing” the pain gate and reducing discomfort. Other treatments, such as acupuncture or massage, work by stimulating specific areas of the body to block pain transmission through mechanisms similar to the pain gate theory. These therapies have proven especially helpful for people dealing with chronic pain, offering relief without the use of medications.
Conclusion
Pain is a complex and multifaceted experience that involves more than just injury. The body has various natural systems designed to modulate pain, whether through the release of endorphins, descending neural pathways, or even mental focus. Psychological factors like stress and relaxation also play a significant role in how we process pain, demonstrating just how intertwined the physical and mental aspects of pain are.
Whether you’re dealing with a short-term injury or managing chronic pain, understanding how your body modulates pain can empower you to better manage your pain. From physical activity to mindfulness and modern pain management therapies, there are many ways to reduce pain and improve quality of life.
By staying informed about these mechanisms, you’ll have a broader understanding of how your body works and the best ways to support it.












